Payment Integrity Teams
Strengthen pre- and post-payment review with AI
Autodor uses AI to process thousands of records and apply clinical reasoning to catch billing issues and overpayments at the source.


Reduce fraud, waste, and abuse
Catch critical issues before and after payment
Traditional payment integrity tools rely on rigid rules to flag coding patterns without a nuanced understanding of the clinical context. With Autodor, our platform detects potential issues before claims are made, effectively shifting the process from post-payment to pre-payment.

Streamline pre-processing
Autodor pre-processes each claim across coding accuracy, medical necessity, itemized bills, and DRG classifications to speed up processing time.
Pre- and post-pay coverage
Missed something pre-payment? Autodor uses the same powerful AI engine to identify overpayments or errors, helping your team maximize recoveries not caught upstream.
Reduce review thresholds
Autodor acts as a helpful assistant for your team, helping you lower dollar thresholds and expand review volume—all without hiring additional staff.
.gif)
Smart triage, real savings
Autodor intelligently categorizes requests based on risk and required expertise. Straightforward cases are routed to fast-track approval, complex cases are routed to the right clinician.
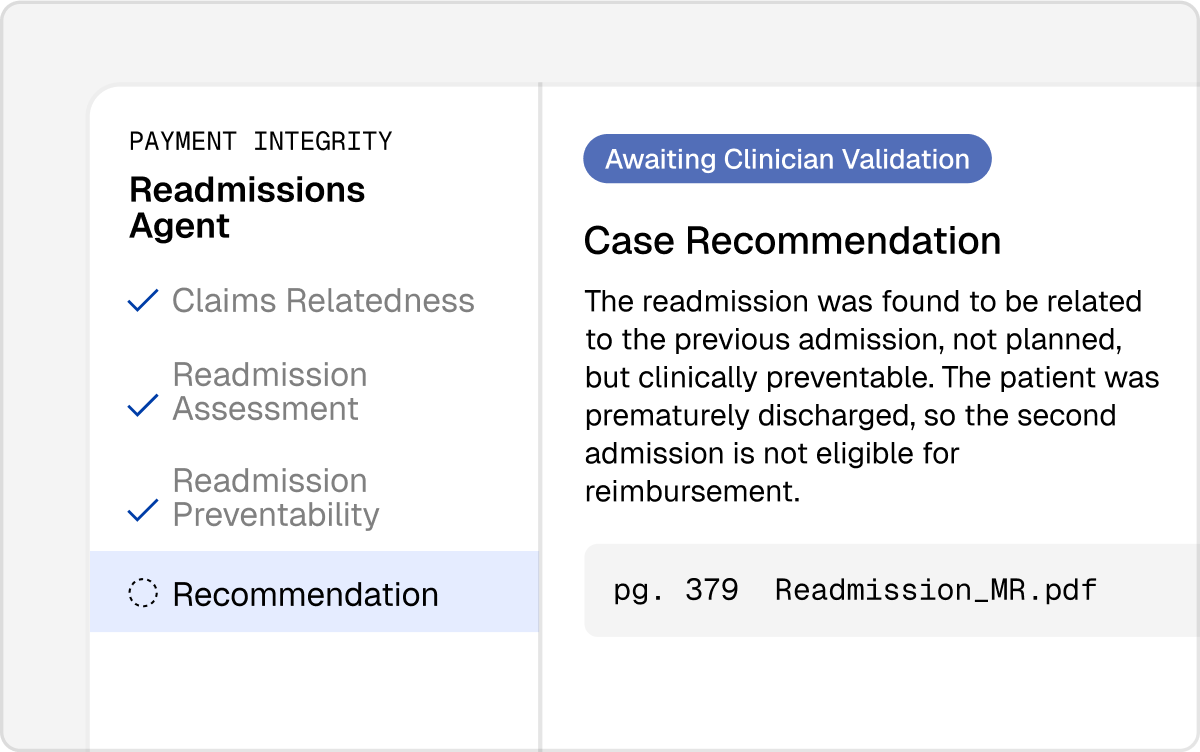
Intelligent clinical reasoning
Autodor clinically reasons against medical records, policy guidelines, and relevant clinical criteria to provide smart, relevant recommendations.
Human validation
Every AI-generated recommendation comes with evidence and policy citations, making it easy for your team to review, validate, and act quickly.
Scale your payment integrity team with Auto Agents
More claims processed. Same headcount. Our custom-built AI agents review coding, billing, and medical necessity, allowing your team to process higher volume with greater efficiency.
DRG Clinical Validation
Medical Necessity Reviews
Readmission Reviews
Short Stays
Itemized Bill Reviews
Flexible engagement models to meet you where you are
InSource
Your clinical team, made better.
Integrate Autodor as a core pillar of your workflows. Your team gains new level of efficiency, productivity, and clarity.
Hybrid
Your team, plus ours.
Combine intelligent automation with in-house and outsourced clinicians to expand scale, consistency, and output.
Outsource
Your claims, our team.
No clinicians on staff? Alaffia becomes your clinical team, pairing expert reviewers with Autodor’s capabilities to handle everything.
Get in touch with a member of our team today to explore which solution is right for you.
Get a Demo"We're excited about using Alaffia's generative AI solutions to streamline our medical claim reviews. We anticipate significant improvements in productivity that will allow each auditor to focus on our highest value work."
Head of Payment Integrity, Regional Health Plan
Frequently asked questions
No. Our pre-payment reviews are designed to reduce friction. Autodor and Auto Agents work behind the scenes to flag errors, inconsistencies, and missing documentation before a denial occurs. We also help health plans implement provider education workflows where needed, so you can build stronger collaboration with your entire team.
Alaffia continuously monitors industry-standard code sets and integrates changes into our platform as they are released. We also review payer-specific policy updates and emerging guidance as it becomes available.
Alaffia’s platform is designed to scale with your health plan’s needs. Our Auto Agents lead to a 20x increase in claims review, supporting everything from high-volume prior authorization to complex payment integrity reviews—all without adding headcount. Because our platform runs in parallel with your current operations, there’s no limit to the number of claims we can pre-process, analyze, and flag for your clinical team.
Boost productivity and eliminate waste
Explore Alaffia on your own, or schedule a demo with a member of our team.


